Breast Cancer Part 4: Reconstruction with Implants
October 30th, 2014
Choices in Reconstruction
Breast cancer is the most commonly diagnosed cancer in US women. Research has found that breast reconstruction contributes to a woman’s self-esteem and sense of wellbeing; however, over 70% of women eligible for breast reconstruction are not told about all of their options. Breast reconstruction generally falls into two categories: implant reconstruction or reconstruction using a person’s own tissue, also known as autologous reconstruction.
We discussed breast reconstruction with fat transfer and reconstruction with flap techniques in previous blogs. Today we will complete our educational series by discussing implant based reconstruction. No matter what your choice, breast reconstruction is inherently staged. This means it will involve multiple procedures, each being one of the stages, to achieve an optimal outcome.
Implant Based
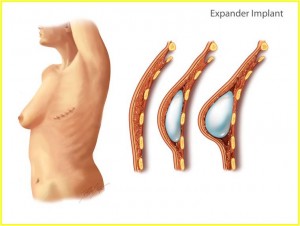
A temporary expander, placed under the pectoral muscle, creates a pocket, which will eventually accommodate a permanent silicone or saline implant. This procedure frequently requires an overnight stay in the hospital and has a recovery time of several weeks. Expansion starts a few weeks after the first surgery after the incisions have healed. The expansion process requires multiple office visits and may take anywhere from two months to one year based on the individual needs and desires of the patient. Once the expansion is complete, the expander is exchanged for an implant during an outpatient surgical procedure. Additional procedures may be required to achieve the desired appearance, shape and symmetry.
Implants are manmade and will eventually fail. Rupture rates are similar for saline and silicone implants and average between 20-25% at 10 years. After 10 years, the rupture rate increases significantly. When a saline filled implant ruptures, your body safely reabsorbs the fluid and the reconstructed breast will flatten as a result. Silicone is a synthetic product and may go undetected when it ruptures. Instead, tissues may become inflamed, causing complications with scar tissue and calcification. When a silicone implant ruptures, it should be replaced promptly. Since silicone ruptures are often silent ruptures, the FDA recommends that women with silicone implants undergo an MRI test three years after having the implants placed and every two years thereafter. This maintenance is an additional personal and financial responsibility for the woman choosing silicone implants.
If you are diagnosed with breast cancer, you have many choices to make so take the time to make the right ones. Immediate reconstruction is safe, but you are not necessarily burning any bridges by delaying your reconstruction for personal reasons. Overcoming breast cancer is a journey and you are not alone. Speak with your primary care physician, breast surgeon and plastic surgeon about your options and help them make the decisions that will give you the best quality of life in the long run. Please click here if you missed Part 1, Part 2, Part 3 of our series.
Photo: Breast Reconstruction with Expander/Implant.
Breast Cancer Part 3: Reconstruction Choices
October 28th, 2014
Take Time to Make the Right Decisions
If you are diagnosed with breast cancer, you have many choices to make. Take the time to make the right ones. Immediate reconstruction is safe, but you are not necessarily burning any bridges by delaying your reconstruction for personal reasons. No matter what your choice, breast reconstruction is inherently staged. This means it will involve multiple procedures, each being one of the stages, to achieve an optimal outcome. Breast reconstruction generally falls into two categories: implant reconstruction or reconstruction using a persons own tissue, also known as autologous reconstruction. Autologous reconstruction can be subdivided into either flap reconstruction, reconstruction with autologous fat transfer or even a combination of the two. All breast surgery will leave visible scars on the chest and although breast reconstruction will rebuild your breasts, the results are variable. Your reconstructed breast(s) will always feel different from your natural breast.
Last week we took closer look at breast reconstruction with autologous fat transfer. This week we will continue our educational series by discussing autologous reconstruction with flap techniques.
Flap Techniques
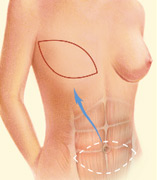
Flap techniques surgically reposition your own skin, fat and muscle to reconstruct your breast(s). Donor sites are areas of your body (abdomen, back, buttocks) where the surgeon harvests skin, fat and muscle for reconstruction. The hospital stay is usually two to five days with a recovery time of several weeks to months. These procedures offer a more natural appearance and feel than that of an implant. However, losing the muscle or part of the muscle from a donor site may leave a residual permanent weakness at that site (abdomen and/or back). You will be left with scars on your chest and another part of your body (abdomen, back or buttocks). Your reconstructed breasts will feel and look more natural but they will not be sensate.
Advances in microsurgical techniques have made free flap procedures available to patients desiring autologous reconstruction. The muscles are preserved during these procedures, therefore reducing the risks of donor site complications and permanent donor site weakness. However, these are lengthy surgeries, requiring specialized expertise in microsurgery and should only be carried out at facilities experienced with the postoperative care of free flaps. Otherwise the morbidity, complication and failure rates can be very high. Flap reconstruction procedures frequently require additional procedures to achieve the final breast contour and symmetry.
Each reconstructive technique has pros and cons. Join us for our next blog about breast reconstruction with implants. Please click here to read previous series Part 1, Part 2.
Diagram courtesy of American Society of Plastic Surgeons